As the number of combat veterans returning home surges, veterans’ treatment for mental health has become a higher priority. For decades, the United States has been in a constant pattern of war, which tends to be linked with lasting mental health issues. Aside from that, the physical injuries many soldiers endure during these wars may have lasting effects on their emotional well-being.
When it comes to veterans’ treatment for mental health conditions, we normally think of post-traumatic stress disorder (PTSD). However, many veterans find themselves facing other problems such as anxiety disorders and enduring depression. Some combat veterans even face uphill battles with traumatic brain injuries (TBI) that have deleterious effects on their mental health.
To combat these and other issues facing veterans today, First Steps Recovery has entered into a strategic partnership with the Veterans Administration (VA) in Fresno, California. A major goal of this partnership is helping veterans break through the stigmas of seeking treatment for psychiatric disorders. With First Steps and the VA on their side, veterans need no longer feel isolated and misunderstood about their mental health.
Empowering Recovery in Veterans’ Treatment: Overcoming Traumatic Brain Injury and Depression
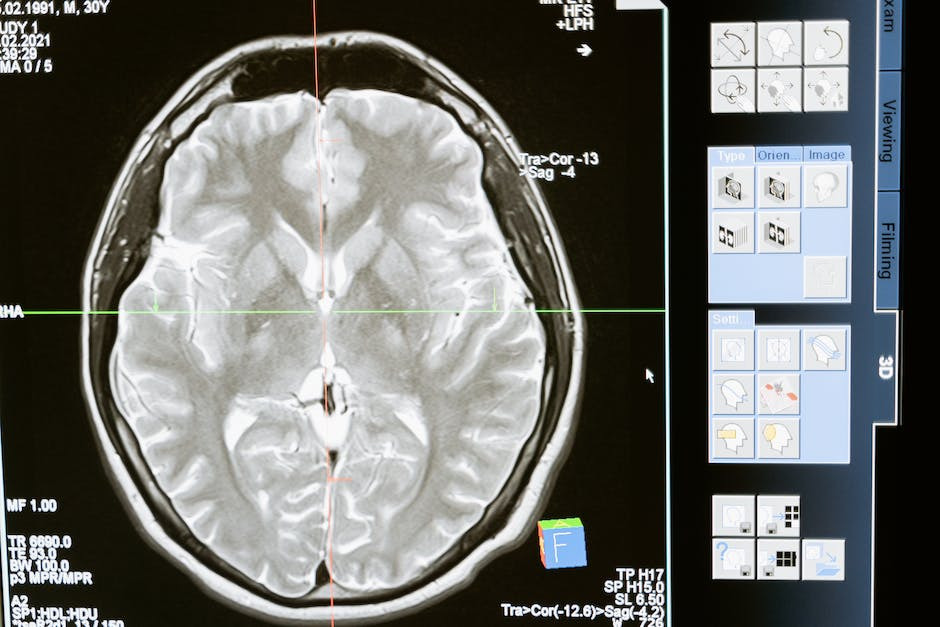
For many people, the term “traumatic brain injury” is unfamiliar. Some people may be more familiar with the term “head injury.” However, it’s all the same. No matter what we call them, these injuries result in serious side effects for those who endure them. Unfortunately, TBIs are often tied directly to the development of depression and other mental health disorders.
Due to the nature of their service, veterans have a much greater chance of enduring TBIs than the average American. Worse still, depression is often not diagnosed alongside TBIs, even when the brain injury is known to be present. Veterans who do not receive a dual diagnosis may not receive adequate treatment for the fallout of their injuries.
Because both TBI and depression greatly affect veterans’ well-being and rehabilitation journeys, dual diagnosis is imperative at the outset. When treatment programs for TBI and depression are integrative, veterans stand a greater chance of recovering from their injuries. This allows them to return to fulfilling and productive lives as private citizens with treatment plans that work for them.
Addressing Traumatic Brain Injury and Depression with Integrated Veterans’ Care
There is a major reason TBIs are often not diagnosed at the same time as the mental health conditions associated with it. A physical diagnosis is often made by doctors who specialize in medicine, while a mental health provider makes psychiatric diagnoses. One conclusion can be drawn from this: There is a need for holistic and integrative healthcare options.
When healthcare is integrated, doctors and mental health professionals can see patterns and connections between conditions. This helps with conditions like TBI, an injury with multifaceted ramifications that extend beyond any one specialty. In comprehensively addressing injuries like TBI, veterans’ treatment plans can include the best care possible.
Recent Issues in Veterans’ Treatment for Traumatic Brain Injury and Depression
In the last two decades of near-constant war, there have been a few lessons learned through experiences with combat veterans. According to the journal JAMA Network Open, scientists have uncovered a link between veteran mortality and the number of brain injuries on the battlefield. In other words, researchers have conclusively linked the development of suicidal ideology with TBIs endured during service.
This discovery allowed scientists to develop evidence-based treatment practices that provide viable treatments for struggling veterans. With the focus on these practices and on tailored interventions, mental health providers can give veterans effective strategies for healing. In doing so, they can effectively counter the potential for suicidal ideology among those suffering from TBIs.
Veterans’ Treatment for Co-occurring Traumatic Brain Injury and Depression
Veterans are used to being self-sufficient people whose wits, determination, and intelligence aid them in foreign environments and on missions. When veterans are grappling with brain injuries affecting every part of their lives, they may not want to seek help. Veterans need to know about caring providers like First Steps Recovery whose mission is to stand beside them.
Residential rehab programs like the one at First Steps provide a safe and secure place to rest while recovering. After years on the battlefield, veterans often require a place to rest where they feel safe and their struggles are alleviated. This inpatient rehab program can cater to the needs of veterans thanks to the resources provided by the VA.
Traumatic Brain Injury, Depression, and Tailored Veterans’ Treatment
No matter who they are, the mental health and physical health journey of every veteran is uniquely intricate and personal. Each person knows their own journey best, and that is no more true than it is for veterans who have returned from fighting in foreign wars. This may make the process of seeking help overwhelming, but the good news is there are veterans’ treatments available.
One therapy offered by First Steps Recovery that has shown efficacy in treating TBI is neurofeedback therapy. These cutting-edge therapies may provide the kind of treatment veterans need to get back up and feel whole again.
Addressing Traumatic Brain Injury and Depression Synergistically
Even when we are alone and feel our most vulnerable, there are networks of caring individuals ready to support us. Many veterans returning home from foreign wars feel the sting of their experience and do not know where to turn. They need direction, and they need to know where they can find help and find answers.
There is hope for treatment of TBI, depression, and other conditions veterans might experience. A holistic consideration of these conditions underscores the interconnectedness within veterans’ mental health and physical health ecosystem.
Two decades of war in foreign lands has taken its toll on the United States and her people. No one has been more affected by the turmoil of these wars than the veterans who have returned home from them bearing the scars of war. When you join the military, you do not expect it to forever change your life with serious and debilitating injuries. However, many veterans have returned home with just such burdens. Often overlooked, traumatic brain injury (TBI) is often comorbid with depression, and veterans disproportionately suffer from both conditions. Thanks to a partnership with the VA, First Steps Recovery offers tailored treatments for veterans. For more information, call us today.